My path from a liberal arts undergraduate education to an emergency medicine residency program—now heading for a fellowship in palliative and hospice care—has been anything but straightforward. Studying medicine has changed me and altered my perception of what it means to be a doctor.
Prior to medical school, I naively thought an inquiring mind was required in solving the mysteries of the human body. Reality was drastically different. Medical school welcomed me with the phrase, “The amount of information you will learn in the next four years will feel like trying to drink water from a fire hose.”
I thought I would think more creatively and feel more like a doctor once my clerkships began and I traded the lecture halls for hospital wards, but my early interactions with patients were skill specific: perfect the physical exam, make the correct observations, and most importantly, practice efficient medicine. The ultimate goal was to secure a good residency position by obtaining high marks. Being a good student meant impressing residents and attending physicians on rounds, checking off boxes, and ensuring that my intern got out on time. I received honors in internal medicine, yet I had trouble remembering the names, faces, and stories of my patients. This bothered me. I wondered whether the character traits that lead to academic success in this environment somehow robbed me of the excitement of caring for patients that first drove me to medical school.
This passion reignited during my residency. The problems I faced in the emergency department were complicated and full of uncertainty. A good memory wasn’t enough. Medicine, I was learning, can be messy. Appreciating the stories of my patients, communicating effectively, and working towards meaningful solutions required curiosity, creative thinking, and analytic skills that had been dormant since I was an undergraduate.
I also recognized pain management as a critical issue, and noted that different physicians have different evaluation and treatment approaches. Physicians are supposed to treat pain based on a scale. Patients are asked to rate their experience from one to ten, with ten being the worst pain. Most patients struggle to choose a number. Pain is a unique, multidimensional, and highly personal experience, yet patients are asked to distill their perception to a number, and physicians must then interpret this number and choose a remedy. The entire process is fraught with subjectivity. The treatment of pain is complicated further by the current opioid epidemic. Doctors balance on a razor’s edge when choosing a treatment: How can they best prevent oligoanalgesia (or the under-treatment of pain) while serving as a judicious gatekeeper to a potentially addictive and lethal class of medications?
This is a dilemma that is multilayered, ethically tricky, and without a simple resolution. I was reminded of the cognitive tools required in studying the humanities. Around the same time, I was fortunate enough to learn of the collaboration between the Brown Emergency Medicine Residency and the RISD Museum. The arts were already changing undergraduate medical education! Students were learning skills to become better observers, to think more abstractly, and to develop greater comfort with uncertainty. This educational opportunity seemed a perfect venue for exploring many complex areas of medicine, including cultural differences, gender, age, socioeconomic forces, and pain.
From this inspiration, I worked with Dr. Baruch, associate professor of emergency medicine and director of the Program in Clinical Arts and Humanities at the Alpert Medical School of Brown University, to develop my project “The Weight of Pain: What Does a 10 on the Pain Scale Mean? An Innovative Use of Art in Medical Education to Enhance Pain Management.” I was fortunate to receive funding from the Department of Emergency Medicine Residency to implement this project in collaboration with the Museum. I worked closely with Hollis Mickey, Sarah Ganz Blythe, and Horace Ballard. They breathed life into my ideas.
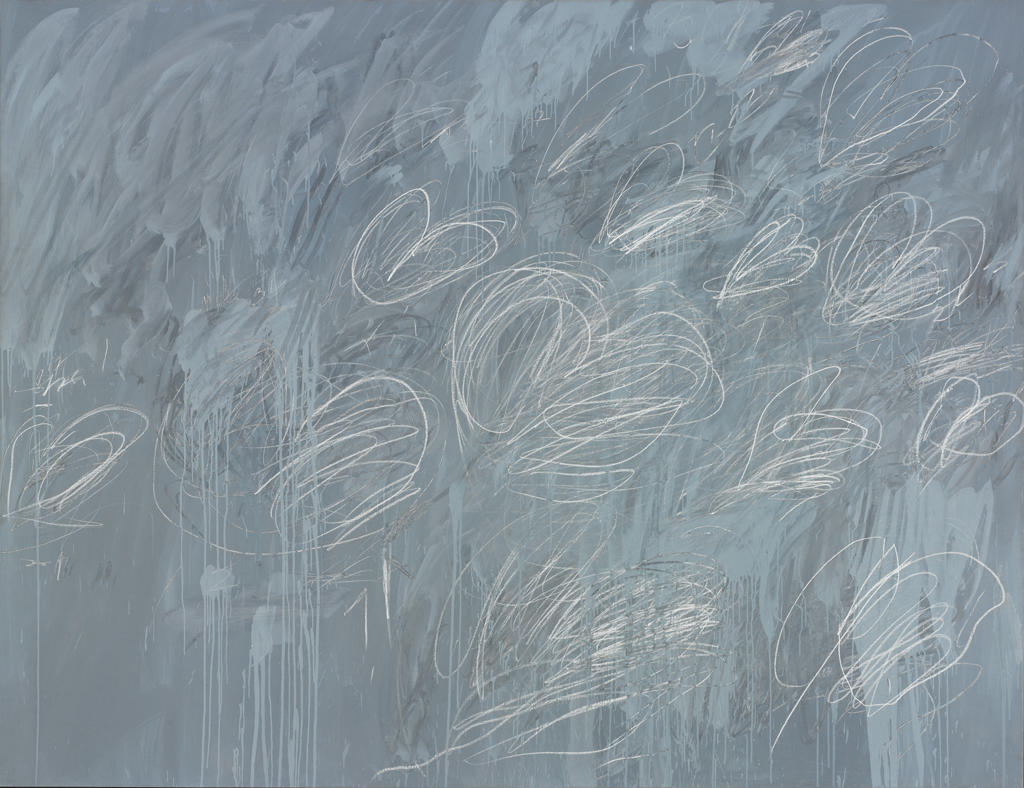
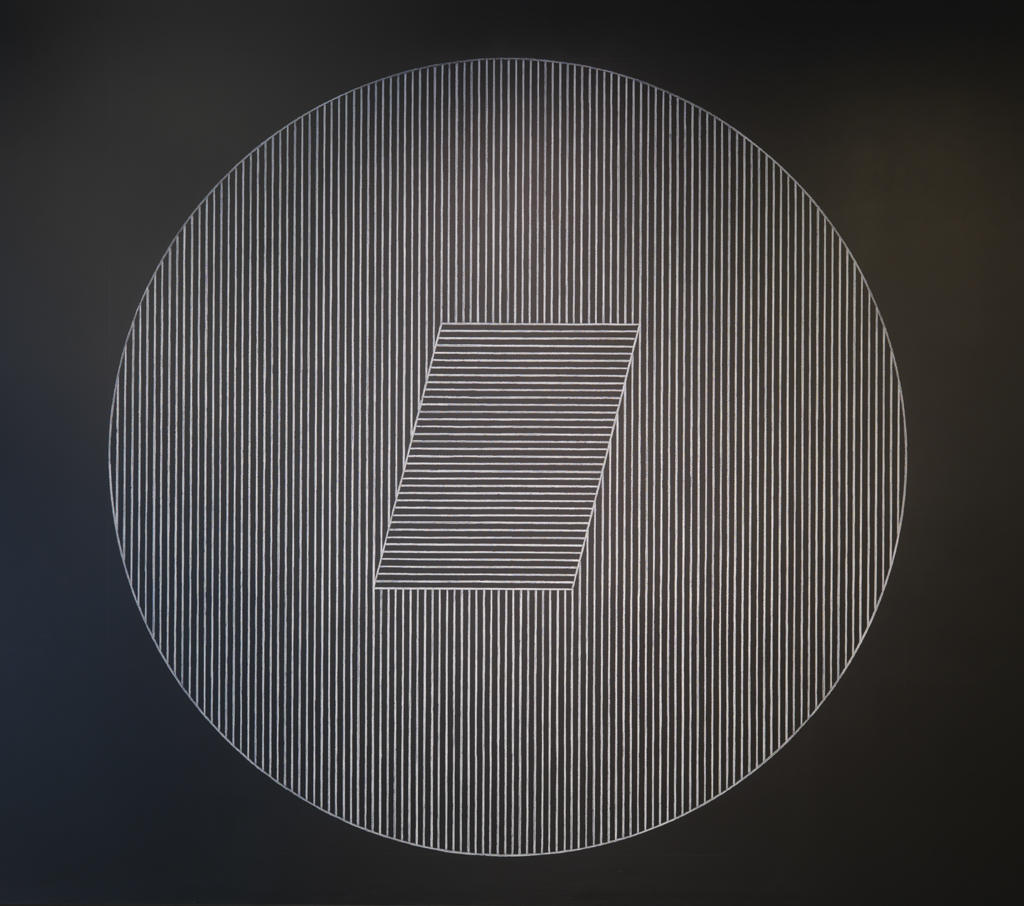
The participants were practicing physicians, both resident and attending, and the initial session required that they spend three hours with one of two pieces. During this time, they made observations and listened to one another as the art educators gradually offered information about the work. I’d never seen my emergency medicine colleagues captivated by one activity! They noted how their observations were made, and how their first impressions were altered by the ideas of other participants. Discussions included how the use of specific words and certain habits of mind can affect pain management.
The success of this exercise prompted my colleagues at the RISD Museum and me us to expand the second session to include internal medicine and palliative care physicians. In this session, participants viewed two works of art. At the first artwork, they were encouraged to formulate a question. At the second artwork, they were asked to answer this question through observations made about this separate and distinct piece. It was exciting to watch participants reflect on how initial impressions can subconsciously seep into their decision-making process. Participants from different specialties all could relate to the difficulties of assessing a patient in pain and being responsible in their management. Afterwards, participants stated the session not only renewed their interest in the topic of pain, but also enhanced their awareness of how they communicate and make observations. One participant wrote that the exercise “reminds us that observation and perception are paramount in the evaluation of our patients.”
The response was overwhelmingly positive. Participants indicated they would be interested in returning for another session and would refer a colleague. Many reflected on how having a better working knowledge of their own biases and cognitive tendencies may affect how they treat their patients’ pain. By bringing physicians back to the humanities in this manner, I hope they are encouraged to analyze their habits of mind and welcome openness in a medical culture that emphasizes thinking and decision-making that’s more formulaic and reductive, and perhaps prone to unconscious bias. I look forward to expanding these ideas in new directions as I begin subspecialty training as a fellow in hospice and palliative care.
Bonnie Marr
MD PGY-4, Emergency Medicine Residency, Warren Alpert Medical School